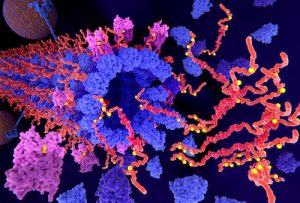
For years, substances called tau protein or beta-amyloid have been theorized to be signs or causes of Alzheimer’s disease. There have been many reports of tests and treatments based on theories that tau and/or amyloid are at least signs, if not causes, of Alzheimer’s. Scientific uncertainty remains about the precise role of tau and amyloid in the disease.
Today’s news about a “breakthrough” test is certainly not the first we’ve heard like that about a possible Alzheimer’s test. On Twitter, former hedge fund manager and TV personality Jim Cramer called it a “major game changer.” Dr. Oz called it a “major breakthrough.” The New York Times headlined its story, ‘Amazing, Isn’t It?’ Long Sought Blood Test for Alzheimer’s in Reach. The story reported:
“Just saying you have amyloid in the brain through a PET scan today does not tell you they have tau, and that’s why it is not a diagnostic for Alzheimer’s,” said Maria Carrillo, chief science officer at the Alzheimer’s Association. By contrast, the tau blood test appears to register the presence of amyloid plaques and tau tangles, both of which are in brains of people with confirmed Alzheimer’s, she said.
“This test really opens up the possibility of being able to use a blood test in the clinic to diagnose someone more definitely with Alzheimer’s,” Dr. Carrillo said. “Amazing, isn’t it? I mean, really, five years ago, I would have told you it was science fiction.”
Note that she said amyloid and tau are both in the brains of people with confirmed Alzheimer’s. Finding both doesn’t confirm whether they are the chickens or the eggs, the cause, or a sign. Cause or association? The Alzheimer’s Association calls beta-amyloid a “prime suspect” and calls tau and amyloid “hallmarks” of the disease.
Eight years ago, I wrote, “Amyloid & Alzheimer’s: the cause-and-effect question that some stories still miss.” As Bloomberg News reported at the time, “scientists aren’t certain whether the (amyloid) clumps cause or are a minor contributor to the disease or merely a consequence.”
Two years ago, we critiqued a Johns Hopkins news release that we felt “prematurely heralds a promising diagnostic tool for Alzheimer’s.” The release described two journal articles that “evaluated ‘tracer’ molecules that might be useful for identifying ‘tau tangles’ — proteins in the brain that occur in patients with Alzheimer’s and other forms of dementia.”
Two years ago, we reported on “rosy speculation about an Alzheimer’s vaccine not yet tested in humans” and how USA Today headlined that it “could cut dementia in half.” The story explained that the vaccine inhibited “buildup of amyloid and tau, two proteins that are hallmarks of the degenerative brain disease.”
Hallmarks of the disease does not necessarily mean that amyloid and tau are causes of the diseases. They may only be surrogate markers. Read our primer on the limitations of surrogate markers.
One year ago, Bloomberg News reported, A Blood Test Can Predict Dementia. Trouble Is, There’s No Cure. Same story this time? Keep reading.
In the first paragraph of the Times story, it describes the findings as “a significant step” with “the potential to make diagnosis simpler, more affordable and widely available.” That is appropriately cautious language. But then the Times projected that “such a test could be available for clinical use in as little as two to three years.” We’ve been down this road before.
And remember, even if the test achieves those goals, how will doctors treat what they find? Eli Lilly, the drug company working on the test, quoted one of the researchers in its news release today:
“Today the majority of individuals with Alzheimer’s disease around the world do not get a timely diagnosis, which results in suboptimal symptomatic treatment and care.”
But The Alzheimer’s Association reminds us of the sober reality – there is no cure for Alzheimer’s disease and no way to stop or slow its progression.
Most of the news stories I saw this afternoon failed to mention this. So we may soon be able to test better. But then what?
Three years ago, when we published, 5 questions to ask when writing (and reading) about new Alzheimer’s drug research, we ended by asking readers to be wary of spreading false hope. That advice, on this topic, still stands today on Alzheimer’s testing and treatment issues.
Because this story broke today, and I’m trying to address some of the early news coverage and social media comments, I will return to add more later if necessary.
-0-
Addendum:
July 29: Susan Molchan, MD, a geriatric psychiatrist and former editorial contributor to HealthNewsReview.org, emailed me her reactions. She first focused on a line from the researchers’ paper, published in JAMA, that stated: “further research is needed to validate the findings in unselected and diverse populations, optimize the assay, and determine its potential role in clinical care.” She wrote:
The major limitations are notes by the authors – to their credit – that the test needs to be studied in a large “unselected” sample, as from primary care clinics. The values that matter are the negative and positive predictive values. It’s also a cross-sectional sample and so we don’t know where/when in the disease course we are measuring this.
Also most dementias are mixed. They are a combo of many different types of pathology ( that’s what aging is!) notably vascular or blood vessel disease. The interactions of vascular disease, amyloid, tau and other proteins and processes is a large area of study.