CELLINK is a 3D bioprinting company based in Gothenburg, Sweden, and was one of the first companies in the world to offer 3D printable bioink, which is used to print human organs and tissues. In just four years of existence, the company has been able to commercialize products used in more than 700 labs and 50 countries. This startup has made a lot of important strides in creating the technology essential to making 3D bioprinting more widespread and accessible to those without the necessary resources. In addition, Cellink has taken a multidisciplinary, tactical approach to conquering tissue bioengineering by looking at the problem bottom-up as well as top-down – from genetics, proteomics, extracellular matrix constituents, and adhesion molecules to scaffold structure, high-fidelity 3D models, and high-level bioengineering.
Having helped create the first 3D bioprinted cornea, CELLINK has also recently come out with the first holographic bioprinter called Holograph X. In 2017, CELLINK’s IPO was more than 1070% over-subscribed and the founder Erik Gatenholm was also placed on the Forbes’ “30 under 30” list in 2018. The company’s acquisition of Dispendix GmbH at the end of 2018 promises exciting additions to their innovations.
I had the opportunity to talk to the co-founders about CELLINK’s journey and technology at the Science in the Age of Experience conference hosted by Dassault Systèmes.

Alice Ferng, Medgadget: It’s very exciting to meet others in the bioprinting/tissue engineering world – tell me about yourselves and what led you to bioprinting.
Erik Gatenholm, CEO & Co-Founder of CELLINK: My background is a bachelors degree in business management at Virginia Tech University, and then a Master of Science in Management focused on innovation and life sciences from the University of Gothenburg. So I’m more on the commercial side and am bringing the technology out to scientists by building the company through marketing sales and management.

Dr. Héctor Martínez, CTO & Co-Founder of CELLINK: My background is in traditional engineering; with a switched focus in bioengineering. Did my engineering bachelors in Texas, then moved to Sweden for a MS in biomedical engineering, and then continued on to get a PhD in tissue engineering, which is when I got into bioprinting.
Medgadget: What was the inspiration behind starting this company? What kind of tissue did you first start working with?
Dr. Martínez: I started with cartilage – auricular (ear) cartilage – and worked a lot with chondrocytes. That was back in 2011.
Mr. Gatenholm: While the concept of 3D bioprinting has been around for some time now, the logistics and challenges behind the technology have so far prevented more complex applications. We started the company with making an universal ink for cartilage tissue since Hector worked with that a lot at his lab. My father was actually his professor, so that was our connection.
At that time, bioprinting had started to come around, but the options were either: buy a bioprinter for $ 200,000 or make one yourself. So we commercialized it for $ 5,000 and we said: everyone deserves to have a printer, especially if you’re changing the world of medicine, and you should be able to do that for a relatively low price. And we understood that it was also all about the material. The material is what drives the cell culturing process, the differentiation, the printed scaffold, or creates the right environment for these cells – the “bioink” is what’s essential. Something else we also understood was that a lot of things could be fixed using software and the right material; the printer is just a tool. It’s a great technology, but it’s just a robot. It needs the right instructions, which comes from the CAD models. That’s essentially why we’re here with Dassault Systèmes; we see the great need of being able to design better CAD models using both AI and machine learning to improve the quality of tissues that we’re printing so that we can make them even more realistic. For example, if we’re printing a piece of the liver – if all of the liver tissue dies after 5 days, we need to decide what is driving that. Is it that the cells are not behaving well in the material? Is it that the model that we are printing is not vascularized? Are the vasculatures in that model too small? Too big? There are a lot of things that come into play to keep the tissue alive.

Medgadget: It’s very difficult to capture the exact native structure and composition of an organ and its microenvironment – which organ or tissue is up next for commercialization (for a non-pharma use case; e.g., implantation)?
Dr. Martínez: It really depends on where the low hanging fruits are. Where we see that are: skin. Skin is a highly complex organ, but there’s a lot of functions that can be mimicked by printing the tissue. We don’t have to mimic every single property of the skin – but can pick the top 3 basics, such as the barrier – keeping the cells both in a humid, but dry environment, and having the right permeability for cells.
Cornea. There’s evidence that bioprinted cornea has a high potential for making it into an implant.
Medgadget: Have you had success with creating and culturing spheroids and organoids? Can you describe what you’re doing here and how you bioprint them?

Dr. Martínez: These have been very successful for pharma applications. We wanted to go from 2D to 3D, and right now we are in the organoid stage. We are using bioprinting to create more complex organoids that are not just one cell type, but multiple cell types with a core and shell of different cell types. We are providing the ability to create these in a reproducible way, and then migrating the organoid technology into bioprinting technology.
The bioprinting itself happens by extruding in a co-axial system having 2 nozzles where you are printing different cell types – 1 for the core, and 1 for the perimeter.
Medgadget: Do you use primary cells or progenitor cells? How are you integrating those into your bioengineering?
Dr. Martínez: Progenitor cells are quite relevant for today’s conversation because we have been doing a lot of work with cell lines. A lot of work has been done in 2D and translated into 3D. But if you want more relative models and more predictive data, then we need to start culturing primary cells. It turns out that primary cells don’t work very well in 2D. And even in 3D models, they don’t live for long; sometimes you can only keep them alive for a few days before they start dying. So what comes into play is a good biomaterial – and what I mean by “good” is that it is specific to the cell type.
We work a lot with cancer researchers and pathologists to understand what is the composition of the tissue and environment. Then we establish the goal and work backwards – we need to have this type of collagen, laminins, specific peptides, proteins, extracellular matrix (ECM), or ECM components that will allow the cells to recognize them as they do in a more native environment. As you had mentioned about your work with matrices in your PhD – these are all key ingredients.
It would be ideal if we could have a completely synthetic material where it is completely chemically defined, but we are far away from that because nature has done a fantastic job at providing just the right environments for the cells. So we are still a ways away from fully mimicking this; but we can learn a lot from nature to identify the key ingredients for cells to behave as they do in an in vivo scenario.
Medgadget: What’s the longest you’ve kept a culture of bioprinted cells alive?
Dr. Martinez: In the latest study, it was about 90 days. In another study we have done with heart cells, we compared culturing primary cardiomyocytes in the traditional way – which died after about 4 to 5 days – with cultured cardiomyocytes that were put in a heart friendly bioink. We were able to keep those cells alive for 28 days – quite a significant improvement.
[This is pretty impressive! That’s long enough to program cells through various differentiation protocols and offers the potential to turn stem cells into specific cell types within a specified niche environment when coupled with the precision of 3D bioprinting technologies.]
Medgadget: What’s next in the lineup of your technology? What are you working on?
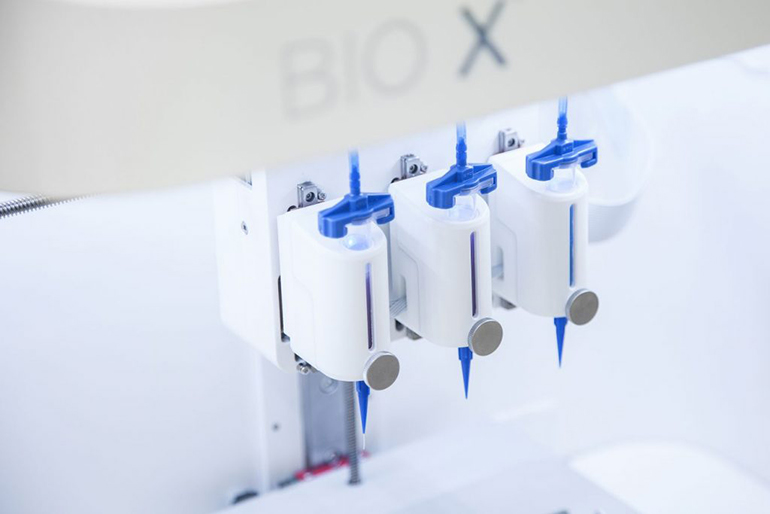
Mr. Gatenholm: CELLINK has acquired a few companies, so there’s a lot in the pipeline. The workflow for bioprinting consists of the following: 1) starting with the blueprint (the CAD model), whether that’s your own design, from a repository, or from your patient (this is probably ideal), 2) then you have your ink and cells – you put your cells inside your ink for a cell-laden biomaterial that you load into your printer, 3) then you load your file, and 4) print out the tissue. And the fourth dimension that a lot of people talk about is the culturing. That workflow is very exciting, but now we are also adding the capability of testing drugs.
We just acquired a company called Dispendix GmbH. They have developed a fast nanoliter dispenser. So it’s a high throughput dispensing system where you can take your printed tissues and put inside the dispensing robot, and dispense compounds. You can see the effect of the compounds on the tissues.
We’ve also recently developed a live cell imaging system, which is a microscope where you can track the tissues over long periods of time. For instance, you can see the effects of a drug over many, many days or weeks. It’s fluorescent-based and integrated with an incubator. Using AI, it counts your cells and looks at cell morphology and behavior and sees if they’re producing the right proteins and things like that. After that, you can compare the data with what you had anticipated – such as your actual tissue with the CAD model to see if there are any differences.
That’s one area. On the other side of our spectrum is the genetics side – DNA and RNA sequencing prior to the bioprinting and creation of tissues. It’s a very wide workflow, but we’re establishing a lot of parts in parallel. It’s very exciting because everyone understands that in order to understand human anatomy outside of the body, you have to go into the 3D environment. You cannot stay in the 2D; it’s already been shown and proven.

Link: CELLINK homepage…
Flashback: 3D Printed Artificial Corneas Seeded with Stem Cells to Alleviate Shortage of Donors
