In the “GET LEAN Eat Clean” podcast above, personal health and wellness coach Brian Gryn interviews Jay Feldman — a health coach and independent health researcher who is extremely knowledgeable in the work of the late Ray Peat — about the underlying causes of obesity and how to optimize mitochondrial energy. I am also scheduled to interview Jay in the near future.
Feldman is the founder of Jay Feldman Wellness and hosts the Energy Balance podcast. A key concept he presents is that when the fuel from your food you eat cannot be efficiently metabolized and converted to energy (ATP), it’s instead typically diverted and stored as fat. In my view, he is the best teacher of Ray Peat’s work. You can view the first seven episodes of his podcast to develop a foundational understanding of bioenergetic medicine.
Another key concept is that high energy production equates to high metabolism, so part of the solution for obesity is to raise your metabolic rate. Unlike conventional wisdom which suggests calorie restriction is associated with longevity, a high metabolic rate slows aging and helps you remain more youthful — at least biologically speaking — as you age.
Lack of Energy Is a Foundational Problem in Obesity
The inefficient burning of fuel (metabolizing of food) is why people who are obese typically also struggle with other health issues, such as low energy, fatigue, an inability to maintain focus, digestive problems and poor immune function.
As noted by Feldman, these all result from a lack of energy production in your mitochondria. So, the primary problem in obesity is that your body cannot efficiently convert the food you eat into energy. Instead, it gets converted into fat. As a result, you end up with obesity, low energy and perpetual hunger, which leads to overeating. Feldman explains:
“I … come from the bioenergetic view of health … the idea that energy, the energy that’s produced in our mitochondria, is the main driver of our health, and a lack of that energy is what leads to dysfunction …
I would say obesity is an energy problem, and endocrine problems are superimposed, happening on the energetic front. So, it’s really helpful to look at hormones … like cortisol … thyroid hormones … the reproductive hormones …
Those things are really helpful when we’re trying to get a gauge on where somebody’s at because you can’t always see what’s happening in the cells and the mitochondria. So, we can look at hormones as a proxy there, but those hormones are just signals and messengers that are being produced or inhibited in response to what’s going on in terms of the energetic state.”
Glucose Metabolism Is Easily Hindered
As noted by Feldman, your metabolism is a sensitive system, especially when it comes to glucose metabolism. Things like mitochondrial dysfunction, psychological stress, oxidative stress (reductive stress), heavy metals, endotoxin, lack of sleep and certain nutritional deficiencies can flip your metabolism into fat burning, which then impedes the metabolism of glucose and converts the glucose into fat rather than energy.
“This is why we want to be looking at food choices in terms of how they affect our energy production,” Feldman says. The conventional view is that fuel equates to energy, which is why obesity is thought of as an energy excess and all you need to do is eat less and exercise more. But that’s not accurate.
“That is something I think we definitely want to work ourselves away from and instead focus on how well we’re using the food that’s coming in, and what types of foods are better used, considering our human physiology,” Feldman says. “That’s really where we want to focus, as opposed to eating less or exercising more.”
Lack of Fat Burning Is Not the Problem
Many, myself included, used to believe that optimizing fat burning was the solution not only to obesity but most other health problems as well, but we’re now starting to realize that this is borne out of a misconception. As explained by Feldman:
“I think what’s happened is we’ve come into this with preconceived notions that people are overweight and have excess body fat, so there must be a fat burning problem. And that is an assumption that I would say is definitely not true …
There have been clear metabolic studies where they see that you can be on a low-carb diet and you can be burning more fat with lower insulin, and having more fat released from the fat stores, and still be losing less body fat because there’s also more fat coming into the fat stores.
And on the flip side, you can be on a higher carb diet, burning less body fat, and still losing more body fat because in that case you’re storing less body fat. So, we’ve just focused in on this one piece of the equation — how much fat are we burning — when it doesn’t acknowledge the whole flow in and out of of the fat stores …
I used to think that … everyone was oxidizing carbs and the problem was that we needed to become better fat burners, but when you actually look at what’s going on in these states, fat burning is part of the problem. That is what happens when things are problematic.
There is one caveat here that’s important, which is that burning carbohydrates doesn’t always mean the same thing. We can oxidize glucose through oxidative processes, meaning we go through glycolysis, and then we go through the Krebs cycle, and then we go through the electron transport chain …
The glucose gets oxidized and we end up with a decent amount of energy. When we are in a degenerated state, in addition to burning more fat, we also run through glycolysis more, and glycolysis is the first step … of glucose burning.
Because there are blocks farther down, we can’t use the glucose all the way, and that’s a problem … but that is not caused by the sugar, it’s not caused by the carbohydrates, it’s not caused by carb burning.
That’s caused by mitochondrial dysfunction caused by our ability to produce energy. So, we’re stuck in a very inefficient glucose burning along with fat burning, and that’s not a great state to be in. But that is not the same thing as fully oxidizing glucose in a healthy metabolic state.”
How Your Body Produces Energy
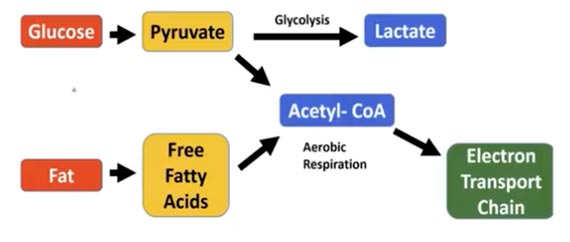
I like to use graphics when explaining this, so let me restate what Feldman is saying, along with a couple of images. In summary, your body can use two fuels for energy: glucose and fat. If you eat any type of sugar or complex carbohydrate, it’s metabolized to glucose. Glucose is then broken down to pyruvate.
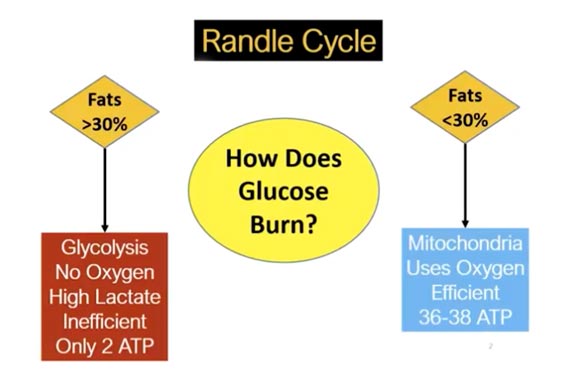
At that point in the process, there’s a “switch,” known as the Randle Cycle. The pyruvate can either enter the glycolysis pathway and turn into lactate, or it can be metabolized into acetyl-CoA through aerobic respiration, as shown in the image below.
Provided your fat intake is below 30% or so (this is merely a best-guess at this point, as
no
one knows exactly what the threshold is), the glucose you consume will be shuttled into acetyl-CoA. When it goes to acetyl-CoA, it goes into the electron transport chain in the mitochondria.
Free fatty acids can also be metabolized into acetyl-CoA through beta-oxidation in the mitochondria, and there’s a competition that occurs there with glucose, which is why your fat intake needs to be low enough for glucose to enter this pathway.
Aerobic respiration uses oxygen in the mitochondria, whereas glycolysis, which occurs in the cytosol, does not use oxygen and is very inefficient. Glycolysis only generates two ATP molecules for each molecule of glucose, whereas aerobic respiration, which occurs in the mitochondria, generates 36 to 38 ATPs per molecule of glucose.
Ultimately, you want to burn glucose in your mitochondria. That’s the most efficient, allowing you to generate the most energy, while simultaneously producing the least amount of harmful “exhaust” in the form of reactive oxygen species (ROS).
And, again, the only way to ensure that is to keep your dietary fat content below 30% of your total calories. If you’re insulin resistant, which means you’re metabolically inflexible, that threshold may be closer to 20% or even 10%. So, if you’re insulin resistant, you’ll want to significantly lower your fat intake until your insulin resistance is resolved. Then you can increase it to 30%.
Endotoxin and PUFAs Decimate Mitochondrial Energy Production
Next, Feldman discusses a key strategy to optimize your mitochondrial energy production, which is to remove blocks in the electron transport chain so that electrons can move smoothly forward, without accumulating and backing up.
“We don’t need to focus on doing extra things to stimulate [mitochondrial energy production],” Feldman says. “Our mitochondria will work perfectly well if they have the right fuel and nutrients, and they aren’t being inhibited or blocked.”
According to Feldman, endotoxin (lipopolysaccharide or LPS) and other bacterial toxins are among the biggest culprits when it comes to things that hinder mitochondrial energy production. These toxins can directly impair electron transport through the complexes of the electron transport chain. They can also impair certain enzymes in the Krebs cycle.
Poor digestion is frequently associated with negative gram bacteria in your gut that produce endotoxin, and this will inhibit your ability to convert food to energy, resulting in increased body fat. So, it’s important to reduce your endotoxin load. Aside from poor digestion, excess endotoxin is also a common culprit in degenerative conditions, metabolic syndrome, diabetes and fatty liver. To reduce your endotoxin load:
- Rebalance your gut microbiome by reintroducing beneficial bacteria (probiotics and prebiotics). One of the best and least expensive ways to do this is to eat a serving of fermented vegetables each day.
- Temporarily go on a low-fiber diet and avoid fiber supplements as it can feed undesirable bacteria. Cook your vegetables thoroughly rather than eating them raw, and if your condition is serious, limit fruits for a time too.
- Eat a low-carb ketogenic diet and/or fast until the problem is resolved. As noted by Feldman, “This is one of the main places where low-carb diets, ketogenic diets, fasting, carnivore [diets] are really helpful, as they provide relief from the feeding of bacteria that are producing a lot of endotoxin.” Foods to avoid include most grains, legumes, nuts, and seeds.
- Avoid resistant starches, as they feed LPS-producing bacteria.
Once your microbiome is balanced and symptoms of poor gut function have resolved, you can slowly reintroduce whole fruits, vegetables, roots and tubers, and other foods. Another effective blocker of mitochondrial energy production is polyunsaturated fat (PUFA).
These are your processed seed oils, canola oil being among the worst of the worst. Seed oils are loaded with linoleic acid, an omega-6 PUFA, which appears to be one of the primary drivers of chronic diseases, in part due to its detrimental impact on your mitochondrial function and energy production.
The Expensive Tissue Hypothesis
After a short discussion about ancestral diets and the likelihood that such diets were generally high in carbs, Feldman and Gryn review the “expensive tissue hypothesis,” which is the idea that the less energy you waste on hard to digest, fibrous foods, the more energy is available for your brain.
“… that’s also a reason to be consuming a lot of carbohydrates and not excess protein, because the conversion from protein to glucose and then to energy is very inefficient,” Feldman says.
“It’s about 30% less efficient than just using glucose. So, if we consider the … expensive tissue hypothesis, we shouldn’t be consuming excess protein beyond our needs and trying to use that for energy, because … that leaves less energy for our immune function, our brain function, for reproductive function and and on …
Coming back to weight loss, there’s the constrained model of energy expenditure, which is very related here, which basically says that you can’t just expend more and more calories from, let’s say, exercise, without it coming at a cost.
So, if you exercise 1,000 calories’ worth and before you were burning 2,000 calories, that doesn’t mean that you just burned 3,000. What actually happens is, you start to cut into your own basal metabolic rate, and you start to cut into your bodily function.
So, your reproduction is turned down, your immune function is turned down … Extrapolated, it really also gets at the problem with the ‘eat less exercise more’ advice for weight loss.”
Endotoxin, Not Fructose, Causes Fatty Liver Disease
Feldman also debunks the argument that fructose, unlike what is being promoted by Drs, Robert Lustig, Richard Johnson and David Perlmutter, causes nonalcoholic fatty liver disease (NAFLD). He reminds listeners that both dietary fat and fructose can be converted into fat, and fructose isn’t automatically destined to end up as liver fat.
“In fact, very little fructose gets converted to fat,” he says, because “there are all sorts of of routes for it to go before it’s getting converted to fat … Fructose does go to the liver and it gets picked up by the liver immediately, whereas glucose will go out into the bloodstream and can be picked up by the muscles.
But our livers have developed to handle massive amounts of fructose. Most of the research that is looking at what happens to fructose … is going on in rats. And there are a few differences, there are a few problems there. One is that rat livers are very different from human livers in their capacity for fructose handling.
Our livers have an incredible capacity for handling fructose. Hundreds and hundreds of grams c
an be stored as glycogen, can be converted to glucose or lactate and sent out to be stored elsewhere, or used elsewhere, and then can also be oxidized.
So, when we consume excess fructose in a normal context, in a healthy liver, very little is going to be going to fat. It takes huge amounts of carbohydrates before you’re … producing much fat in the liver through de novo lipogenesis. And that’s because our livers have this incredible capacity for handling it …”
Feldman also remarks that many fructose studies are flawed in that they’re looking at fructose-only sources, which rarely ever exists in our food supply as it is virtually always accompanied with glucose. Results from such studies therefore do not tell you much about how natural, whole food-based fructose, say from fruit or honey, acts in the body.
“Whether you’re consuming fruit or honey or anything else, the fructose to glucose ratio is always near 1-to-1,” he says. “Sometimes there’s a slight bit more fructose [than] glucose, but even in high fructose corn syrup … it’s about 55% fructose and 45% glucose. We’re really not talking about major differences here.
And that’s important because our intestines don’t absorb pure fructose. If there’s glucose present, we absorb it very well. But if there’s no glucose present … you can’t really absorb it very well.
So, what happens is a lot of it doesn’t get absorbed in our small intestine. [It] continues down to the large intestine where it feeds bacteria. Those bacteria produce endotoxin, and that is what leads to things like fatty liver production [and] fatty liver disease.”
How to Gauge Your Metabolic Rate
According to the rate-of-living theory, the higher your metabolic rate — which means the quicker the electrons move from food toward oxygen, which is the final acceptor of electrons — the faster you’ll age because there’ll be higher oxidative stress.
However, deeper analysis reveals the exact opposite. The truth is, the higher your metabolic rate, the slower you age, because a high metabolism creates fewer ROS that can damage your tissues.
Your metabolism is high when electrons move rapidly and easily through the mitochondrial electron transport chain, which results in optimal energy production. When electrons are impeded from moving forward, they can back up, leak through the mitochondrial membrane and start moving backward, where they combine with oxygen to create excessive ROS.
So, for optimal health, you want high energy production and that means a high metabolic rate. As explained by Feldman, you can gauge your metabolic rate using your pulse and body temperature.
“If you’re not hitting 98.6 [degrees Fahrenheit] later in the day, if you’re not hitting 97.8 or 98.0°F when you’re waking up, that can be a sign of a hypometabolic state,” he says.
“If your [resting] pulse [first thing in the morning] is particularly low, if you’re not getting into the mid-70s or potentially low-80s, depending on your fitness state, that can also be a sign of a low metabolic rate.
The caveat is that the more cardiovascularly fit you are, the lower your pulse rate will be, independent of metabolic state. That’s because your stroke volume increases. The stroke volume is the amount of blood your heart pumps with each beat. So you can have fewer beats and still pump the same amount of blood … You can also look at temperature and pulse before and after a meal.
If … somebody wakes up at temperature 98.4°F. and then they have their breakfast and it drops to 97.5°F., that is a situation of a drop in stress hormones, where someone was waking up in a stress state, their sleep’s probably not optimal, they’re probably not optimal metabolically, then they’re consuming some carbohydrates and their stress hormones drop.
If you’re seeing that happen after a meal, it’s a pretty good sign that that’s what’s happening.
Another good way to do it is just seeing how many calories you can consume while maintaining your weight … If, with your activity and everything else, you should be burning 3,000 calories a day, but you’re maintaining your weight on 2,200 calories a day, that’s a sign that you’re pretty hypometabolic.”
Conversely, if you can maintain your weight when you add more calories, your metabolic rate is likely high, and the extra food will oftentimes improve your sleep, relaxation, energy and recovery.
Methylene Blue — A Useful Rescue Remedy
While there are no magic pills to fix slow metabolism or low energy production, there are some that can help. I’ve previously written about the usefulness of niacinamide, for example. Another helpful one is methylene blue. As explained by Feldman:
“As a supplement, it’s got a number of interesting effects. For one, it’s antimicrobial … but it also has some pretty interesting mitochondrial or energetic effects, where it is able to work as an electron acceptor and donor.
So, if things are not working well in the electron transport chain, the main site where we produce ATP, [if] something’s blocked, let’s say by endotoxin or polyunsaturated fats, whatever it is, methyl blue can help us bypass those issues and allow us to continue to produce energy despite those things.
It also lowers nitric oxide, which is another inhibitor of mitochondrial respiration. So, it’s got a number of benefits. I will say, like any other supplement, there’s a place for it and there’s also a place where it can be problematic, and it’s never the first thing I would go to.
We always want to work at those foundations first — get diet on point, eat consistently, get enough carbs and fats in, make sure we’re getting the nutrients we need, trying to work on our sleep hygiene, our movement …
But I do think there’s a place for methylene blue to help with either those microbial issues or for getting the metabolism going in certain instances. It also, in particular, has some benefits neurologically, because of these stimulating effects on respiration … So, yeah, I like it. Again, it’s not magic in that it is going to fix the problems, but it can be helpful along the way.”
Constructing the Ideal Diet to Maximize Energy
While it’s nearly impossible to come up with a diet that is ideal for everyone, general guidelines can be provided. After that, it’s up to you to experiment and note what works and what doesn’t. For example, some are outfitted with genes that can handle dietary fats better than others, while some may have had their gallbladder removed and can’t handle much fat at all. Following are some general principles for devising your ideal diet:
• Protein — Most adults need about 0.6 to 0.8 grams of protein per pound of lean body mass. As an example, if your body fat mass is 20%, your lean mass is 80% of your total body weight. Ideally, stick to animal-based protein such as clean seafood and low-LA animals like beef, bison, lamb and other ruminant game animals, raw grass fed dairy and organic pastured eggs.
Avoid chicken and pork as, even if pasture-raised and organically fed, they are given grains and other foods that are high in LA so they will increase your LA levels. Many plant-based proteins, including nuts and seeds (with the exception of macadamia nuts), are also
high in PUFAs.
• Carbs — Avoid hard-to-digest carbs like most grains, including brown rice, and legumes, unless they’re soaked, properly cooked, sprouted or fermented. Good options include raw authentic honey, maple syrup, white rice, ripe and dried fruit, and well-cooked (preferentially pressure cooked) tubers like red potatoes, sweet potatoes and parsnip.
• Fats — Avoid seed oils, which are loaded with PUFAs like LA. Good options include butter, tallow, ghee, coconut oil and avocados.
If you’ve been on a low-carb, high-fat diet, slowly add in more carbs while simultaneously lowering your fat intake. As mentioned earlier, your fat intake probably needs to be somewhere around 30% or lower to allow for efficient glucose metabolism.
Feldman typically recommends a range of 20% to 40%, with the upper limit being for more physically active people with greater muscle mass. With fats at 30%, carbs would then be in the range of 55% to 60%, with protein making up the remaining 10% to 15%.
Increase Your Metabolism to Slow Your Aging
As mentioned earlier, high metabolism is the key to slowing down aging. And the slower you age, the more youthful and resilient you’ll be. As noted by Feldman:
“When we’re in our 20s, let’s say, or late teens, we can kind of eat whatever, our metabolic rate’s really, [we have] high libido’s, sleep is never an issue … digestion is really good; things don’t bother you. That’s the state … we want to be getting to. And I would say the key difference there is, where is our metabolic rate at?
Over time, metabolic rate slows, mitochondrial respiration slows. If you take aged mitochondria from someone who’s above the age of let’s say 60 or 70, there’s a dramatic reduction in energy production … So, the solution is to get back to that young metabolism. And I think it’s totally doable.
It’s just a matter of eating the things that are designed for optimal function, that allow for maximal energy production, [and] avoiding the things that interfere with that — avoiding the polyunsaturated fats, lowering endotoxin, having good, consistent sleep, consistent movement.
It’s a complex, right? It’s never as simple as ‘Just eat this one thing,’ or ‘just take this one pill.’ [It’s] having that perspective of trying to think of speeding things up, as opposed to slowing things down.”
