What if your human cancer cells do not undergo apoptosis, but simply continue to divide and grow? Although we frequently think residing all the time might be extraordinary, it is not great when it happens in your cells. When the damaged cells divide continuously and do no longer undergo normal apoptosis, the result is most cancers.
Apoptosis and cancer[1] are connected in some aspects. First, tumors cannot grow if the system’s normal security within the body detects and actively self-destructs. Cancers often block the mechanisms by which the body marks the growth of uncontrolled tissue for apoptosis. Second, cancer cells inactivate the genes encoding the proteins necessary to destroy malignant cells in some organ cancers like lung cancer, liver cancer or pancreatic cancer.
Even though many things go wrong to turn a new cell to be a cancer cell, one of the most essentials is the deregulation of the process of apoptosis. Cancer occurs when tumor cell division out of control and the mechanisms that regulate apoptosis stop working. The tumor cells divide unexpectedly, invade, and displacement of normal healthy tissues and organs.
The Apoptosis Pathway
Apoptosis is triggered by various agents, including endogenous cytokines, therapeutic drugs, and cytotoxic. Initiation and implementation are mediated, in many cases, by activation of caspase family members of specific cysteine protease-aspartate.
If the cells are damaged , they commit to preventing themselves from becoming harmful to the body as a whole. The cells with DNA damage, for example, can become cancerous, so they should commit apoptosis before that can happen.
Apoptosis pathways[2] the so-called extrinsic pathway of apoptosis or death receptor pathway, involving the killing of tumor cells initiated by cytotoxic T lymphocytes. The other major signaling pathway leading to apoptosis is the mitochondrial or intrinsic apoptotic pathway.
This pathway is regulated by the BCL 2 family proteins[3], which manipulate the intracellular environment of mitochondrial integrity. BAX and BAK are BCL 2 family members that induce cell death by drilling holes in the outer mitochondrial membrane death which leads to the release of mitochondrial proteins in the cytoplasm, where they activate caspases.
Intrinsic Mitochondrial Apoptosis Pathway
Intrinsic Mitochondrial Apoptosis activates when the cell is stressed by a series of factors, including DNA damage exposure to UV light and X-rays; hypoxia; accumulation of misfolded proteins within the cell and chemotherapeutic agents induces apoptosis, for example, Huntington’s disease, Alzheimer’s disease, and Parkinson’s disease. When the cell is stressed, a leak of cytochrome c releases intermembrane space of mitochondria into the cytosol leading to activation of caspase 9. TP53 and Bcl-2 family genes regulate this pathway.
Extrinsic or Death Receptor Pathway
The extrinsic pathway[4] is triggered when the cell perceives the death of the other cell signal. The extrinsic pathway is linked to receptors and related apoptosis inducing ligand binding to other cells of the death receptors on the cell surface. It then leads to activation of apoptosis pathway. As a result of binding, this involves the following signaling complex inducing death (DISC) a cell surface receptors and respective ligands, resulting in the activation of auto-catalytic procaspase-8. When caspase-8 is activated, the execution or terminal phase is triggered:
- TNFR activated by cytokine TNF: TNF-alpha is a cytokine produced by macrophages and is the primary mediator of extrinsic apoptosis. Tumor necrosis factor (TNF-alpha) binds to receptors TNFR1, leads to caspase activation.
- Fas (CD95) receptor activated by FasL (Fas ligand): The Fas receptor is a transmembrane protein of the TNF family that binds Fas ligand (FasL). The interaction between FasL and Fas receptor L leads to caspase activation.
Cytochrome C Role and Genetic Mitochondrial Apoptosis Regulation
When the cell is stressed out from the inside, the role of the Bcl-2 protein that regulates the permeability of mitochondria in response to apoptotic signals comes in and the release of cytochrome c[5].
TP53 Suppressor Gene
This gene encodes a p53 protein that controls the cell cycle death and causes the tumor suppressor gene. If the DNA is damaged, for example, chemotherapy agents, hypoxia, or by ionizing radiation. The T P53 gene stops the cell in the G1 phase of the cell cycle and prevents the proliferation of the cells with DNA and the DNA repair damage. But if DNA damage is too largeit will promote cells by activating the apoptotic gene BAX. BAX gene BCL 2 products then deactivate anti-apoptotic genes.
Bcl-2 ( b cell lymphoma) Family of Genes
Located on chromosome 18, it is anti-apoptotic genes in that they produce the Bcl-2 expression protein. Bcl-2 binds to and inhibits Apaf-1, thereby preventing the release of cytochrome c from mitochondria. Cytochrome c is present between the outer and inner mitochondrial membranes. Upon release, Apaf-1 binds to and activates pro caspase 9.
Perforin / granzyme
In some cases, immune cells called cytotoxic T cells can initiate apoptosis. This occurs when lymphocytes secrete a protein called perforin and small particles containing specialized enzymes. Perforin[6] holes created in the plasma membrane of the target cell. Additional particles for use holes enter the cell. After entering the cell, they release their enzymes (granzymes A and B) that the execution path begin
s and wreak havoc on cell structure and function.
The Role of Apoptosis in Cancer cell
Before apoptosis is discovered, proliferation, differentiation, and senescence have been understood as the only process that controlled cell populations. In contrast, there was evidence of another form of cell death.
Apoptosis plays a vital role in controlling the cell populations. The inability of cells to undergo this process can have dramatic consequences, depending on the cell type.
Today, apoptosis is known to play an essential role, such as:
- Maintaining a particular number of cells in an organism – With mitosis to provide more than 100,000 cells within the human body every second, other cells die by apoptosis, thereby maintaining a constant number of cells present in the body.
- Homeostasis – As the B cells and T cells of the immune system and the intestinal epithelium produced in large quantities . In the case of B and T cells, the greater number of die 95 percent during maturation by apoptosis. Here, apoptosis plays an important role in the control and balance of the cells to prevent autoimmunity.
- Get rid of redundant and damaged cells – In the body, cells damaged significantly that cannot be repaired are eliminated through apoptosis. This also happens to the infected cells and auto-reactive immune cells.
Induce Apoptosis can lead to new Cancer treatment
Researchers from the Hebrew University of Jerusalem and the Weizmann Institute of Science have developed a technique to cause apoptosis, or programmed cell death, that could lead to new approaches to treating cancer.
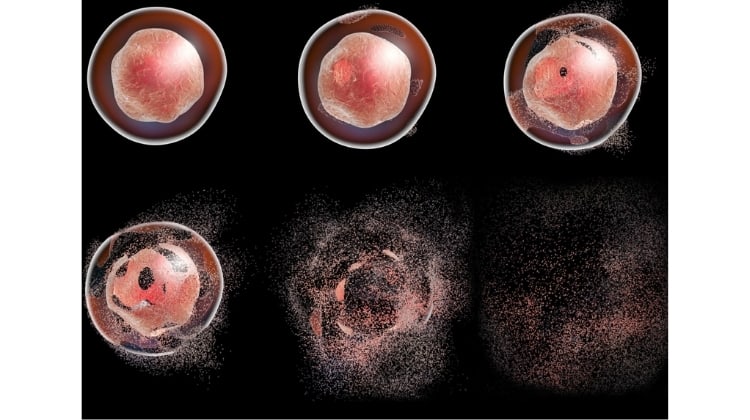
The study examined the interaction between two important proteins involved in cell death: mitochondrial carrier homologue 2 (MTCH2), which was discovered in the lab of Prof. Gross, and truncated BID (tBID), which are both involved in the apoptotic process. The researchers found the regions in the two proteins that are responsible for binding to each other, a critical step in initiating apoptosis. Following their discovery, the researchers developed short synthetic protein fragments, or peptides, that mimicked the areas on the proteins that bind to each other, and by doing so inhibited this binding. In lab experiments conducted on cell cultures, this resulted in the death of cancer cells of human origin.
”These protein segments could be the basis of future anti-cancer therapies in cases where the mechanism of natural cell death is not working properly,” said Prof. Friedler. ”We have just begun to uncover the hidden potential in the interaction between these proteins. This is an important potential target for the development of anticancer drugs that will stimulate apoptosis by interfering with its regulation. ”
apoptosis in cancer treatment
In contrast, Tumor cell death[7] by cancer therapy commonly used in cancer treatment such as chemotherapy, γ-radiation, immunotherapy, or gene therapy suicide predominantly mediated activation of apoptosis, the cell death program intrinsic. Therefore, defects in apoptosis pathways can lead to resistance to cancer with current treatment approaches. Understanding the molecular mechanisms that regulate cell death programs, including apoptosis, and how resistant forms of cancer evade apoptotic events, can provide new opportunities for the development of cancer drugs.
Cancer therapy, chemotherapy drugs, and radiation workforces a cancer cell to undergo apoptosis triggering cell death signals causing trouble or damaging DNA. Moreover, many drugs that induce apoptosis are currently being investigated, and some clinical trials are. In addition, a cancer cell in favor of the death BH3 proteins accumulate but do not exert effects strong enough to overcome excess protein Bcl-2 anti-apoptotic proteins.
Drugs that mimic BH3 proteins can give an extra boost to strengthen the pro-death signals, causing the intrinsic pathway forward and causing apoptosis. Several agents being tested directly target the anti-apoptotic protein Bcl-2 family and IAP, and several pro-apoptotic factor returns that have been eliminated, such as caspases or p53 protein gene function.
In contrast, there are many ways a cancer cell may prevent apoptosis. While drugs can target and restore apoptotic pathways, cancer cells become resistant and can acquire new mutations. For example, if a drug inhibits the proteins of the Bcl-2 family, it will initiate apoptosis in normal cancer cells, as well as cancer stem cells. But if they then acquire a mutation that upregulates caspase inhibitors, the drug will be more effective.
Frequently Asked Questions
Apoptosis is programmed (to maintain normal in the organism), while necrosis is due to external factors such as injury or toxins. Apoptosis is controlled so that the cells are not needed or potentially harmful eliminated.
Apoptosis caused by proteolytic enzymes called caspase 3, which causes cell death by cleaning a specific protein in the cytoplasm and nucleus. Sometimes cells also damage or stress so that they can kill themselves by triggering and activation of procaspase aggregation in the cell.
There are three apoptosis known pathways in these cells, i.e. the extrinsic pathway, the intrinsic pathway and Perforin / Granzyme Pathway.
Apoptosis or programmed cell death is a natural phenomenon by which our body cells are killed after their useful life is over. But in the case of cancer cells, apoptosis is not functional, so they do not die and continue to divide and form piles of cells we call tumor.
NK cells are a type of lymphocyte responsible for granulated cytotoxic to induce apoptosis in the “defective” cells. Their granules contain granzyme that opens the pores in the cell membranes to kill the labeled cells and associated molecules required for apoptosis in the cell.
Apoptosis is programmed cell death autolysis is then digestion of the cell to the inside. Autolysis is a response to injury or infection, and generally does not occur in healthy cells, while Apoptosis can be a process in healthy tissue
